If your eyes are bothering you, it is very important to have a thorough eye examination to properly diagnose the cause(s). If you have more than one condition (e.g. dry eye, allergies, blepharitis, ocular rosacea, meibomian gland dysfunction (MGD), contact lens related issues, conjunctivochalasis, demodex, other) it is imperative that each is identified. This is because treating only one condition will be met with limited success. Your eyes and eyelids will be their healthiest when all conditions causing irritation and inflammation are properly identified and treated.
Meibomian Gland Dysfunction (MGD) is a chronic, diffuse abnormality of the glands in your eyelids known as meibomian glands. Meibomian gland dysfunction is often associated with blepharitis*, ocular rosacea**, and/or demodex*** (see definitions below).
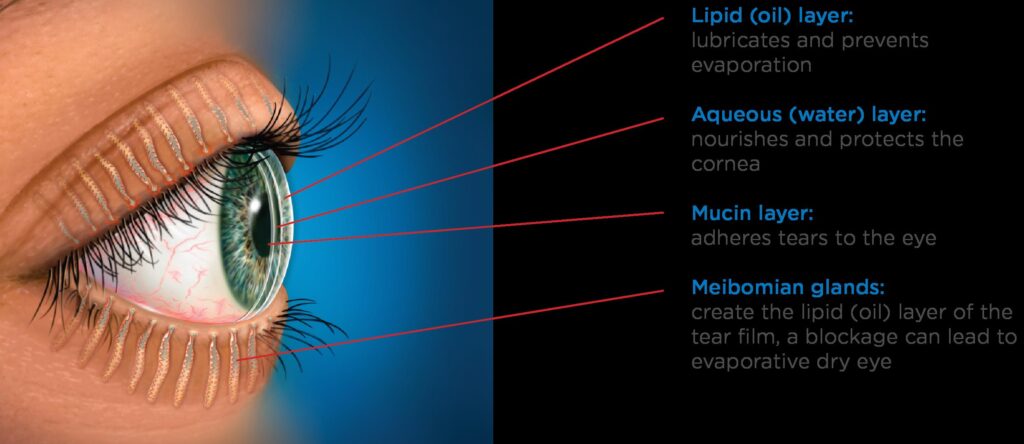
The meibomian glands are oil producing glands in both your upper and lower eyelids. The oil produced by these glands forms the outermost layer of your tear film. This oil layer protects your tears from rapidly evaporating. When these oils are reduced or eliminated, your tears evaporate from the surface of your eyes quickly and your eyes become much drier. This is especially true when you are engaged in visually intense tasks such as reading (books, magazines, newspapers), staring at a computer, cell phone, or tablet screen, watching television, driving, etc.
When the meibomian glands are healthy, the oil they produce has the consistency of olive oil. When the glands are inflamed, the oils they produce become thickened, having a consistency more like that of toothpaste, leading to clogging of your meibomian glands. When your meibomian glands become clogged, the oil layer is not contributed to your tear film; your eyes become drier, and more irritated and inflamed. This inflammation causes damage to the surface of your eyes and your tear producing glands. Additionally, the back pressure caused by the clogging of your meibomian glands results in damage to the glands, with gland shortening, atrophy and death.
Untreated, meibomian gland dysfunction is chronic and progressive. Allowed to progress, the damage to meibomian glands is irreparable and can lead to significant discomfort with dry, red, irritated and inflamed eyes, recurrent infections, scarring of the surface of your eyes, and decreased vision.
Unfortunately, lost meibomian glands do not have the ability to spontaneously regenerate.
Blepharitis, ocular rosacea and meibomian gland dysfunction are very closely related. They all cause damage to your meibomian glands secondary to inflammation, thickening of the meibomian glands' contents, clogging of the glands, decreased oil production, and the accumulation of a biofilm****on your eyelids.
Routine screening and evaluation are essential for early detection and intervention to prevent Meibomian gland loss.
There are Subsets of Meibomian Gland Dysfunction, Blepharitis, and Ocular Rosacea
There are different types, forms, or subsets of Meibomian gland dysfunction (MGD), blepharitis, and ocular rosacea:
1. MGD, blepharitis, and/or ocular rosacea with clogging.
2. MGD, blepharitis, and/or ocular rosacea with mechanical obstructions.
3. MGD, blepharitis, and/or ocular rosacea with both clogging and mechanical obstructions.
Clogged (inspissated) Meibomian glands are distinctly different from mechanically obstructed Meibomian glands, and the importance of making the correct diagnosis cannot be overstated. Knowing whether you have one, the other, or both is imperative because the treatment needed to resolve each condition is different.
Specifically defining which (if any) subset of these ocular surface conditions you have can benefit you by providing the opportunity to create a treatment plan that is precisely tailored, customized, and targeted to your individual needs. This has been shown to result in the best outcomes. For example, if you have an obstructive component to your MGD, blepharitis, or ocular rosacea and are unaware of it, you miss the opportunity to treat it properly.
Subsets of Meibomian Gland Dysfunction, Blepharitis, and Ocular Rosacea Explained
There is a distinct and very important difference between Meibomian gland clogging and physically/mechanically obstructed Meibomian glands, referred to as “obstructive Meibomian gland dysfunction”, or OMGD.
One hallmark of MGD, blepharitis, and ocular rosacea is clogging of the Meibomian glands. This occurs when the oils produced by the glands—normally flowing like olive oil—become thicker or more viscous, similar to toothpaste or lard. The thickening causes the gland contents to clog, inspissate, or congeal. This clogging results in back pressure that stresses the glands, causing them to shorten, atrophy, and ultimately be lost.
These cases can typically be managed with natural remedies, medications, at-home heat application, and proper lid hygiene, often followed by an in-office deep-heat treatment known as LipiFlow, iLux, or TearCare. These treatments comfortably apply heat and pressure to liquify and express the solidified contents of the glands, thus cleaning them out. LipiFlow, iLux, and TearCare are extremely effective at melting and clearing clogged material—unless intraductal or periductal mechanical obstructions are also present.
Many individuals with MGD, blepharitis, and ocular rosacea have an additional mechanical obstructive component. This is primarily the result of chronic (months to years) inflammation of the eyes and eyelids. Ongoing inflammation leads to fibrous or fibrovascular scar tissue forming inside the glands, physically obstructing the ducts or pathways.
Additional factors contributing to Meibomian gland obstruction include:
• Accumulation of keratin contributing to gland narrowing or blockage
• Dead skin (epithelial) cells and debris can build up and obstruct the glands
• Eye rubbing due to allergies, causing trauma and worsening inflammation
• Makeup residue (eyeliner, mascara), especially when placed near or on the waterline
• Decreased blink rate from prolonged screen use or contact lens wear, leading to stagnation of gland contents
Obstructive MGD can include fixed intraductal mechanical obstructions (cellular debris, fibrosis, granulation tissue) or periductal fibrosis, blocking the gland ducts or pathways. These blockages obstruct oil flow, creating increased pressure behind them. This can cause tenderness, inflammation, gland shortening, atrophy and loss, recurrent eyelid infections (styes, hordeola, chalazia, cellulitis), and classic symptoms of ocular irritation.
Obstructions may occur at various points within or outside the glands, allowing some glands to be partially functional while others are completely blocked. This is why some glands may produce a little oil, but still not be healthy.
Standard first-line treatments and in-office heat procedures used for traditional MGD cannot adequately treat fixed mechanical obstructions. These obstructions must first be removed or released for relief and to halt progression of disease. This is when Meibomian gland probing becomes appropriate, indicated, and invaluable.
If Meibomian gland obstructions are not mechanically cleared, the condition will progress. Symptoms may be episodic, but even intermittent irritation, inflammation, and pressure can result in cumulative, irreversible gland damage.
For More Information Regarding How to Diagnose and Treat Obstructive Meibomian Gland Dysfunction please go to this page: https://dryeyespecialist.com/treating-mgd/
Terms Defined
*Blepharitis:
Blepharitis is a condition where there is inflammation of the eyelids around the area of the eyelashes and the meibomian glands. You can have a seborrheic component (often with "dandruff" in your eyelashes) and/or a bacterial (staphylococcal) component sometimes causing styes or chalazia.
**Ocular Rosacea:
Ocular rosacea is characterized by inflammation of the eyelids. It is often the first sign of rosacea of the face (which can involve the nose, cheeks, forehead and chin). People with rosacea tend to blush or flush easily. People with rosacea also have a much higher incidence of Demodex infestations.
***Demodex:
Demodex mites are little bugs that can infest your eyelashes, eyelash follicles and eyebrows. These mites are nocturnal, coming out of your eyelash follicles at night to eat, mate and lay their eggs. Their life cycle is typically 2 to 3 weeks. If your eyelashes are infested with Demodex you may experience redness, itching or irritation of your eyelids, "dandruff" in your eyelashes; while some people with demodex are unaware of any symptoms at all. Demodex infestations cause damage to your eyelash follicles and your meibomian glands, making it important to quickly diagnose and treat an infestation.
****A biofilm is a slimy, sticky film of bacteria that coats the surface of the eyelids. A biofilm is composed of a well-hydrated matrix of bacteria and their glycocalyx, a sugary coating that allows cells to adhere to and communicate with each other. The eyelid margin with its moisture, nutrients and warmth, is the perfect environment to cultivate a thriving bacterial biofilm. Some people experience an increased frequency of accumulation of a tenacious biofilm along their eyelid margins. These individuals benefit from periodic exfoliation of their eyelids to keep their meibomian gland orifices (openings) uncapped of unclogged. This helps to ensure the health of the meibomian glands, and decrease irritation and inflammation, thus keeping the eyes and eyelids healthier and more comfortable.








